IASbaba's Daily Current Affairs Analysis, IASbaba's Daily Current Affairs June 2016, International, National, UPSC
Archives
IASbaba’s Daily Current Affairs – 14th June, 2016
INTERNATIONAL
TOPIC: General studies 2
- International relations – India and its neighborhood- relations.
- Bilateral, regional and global groupings and agreements involving India and/or affecting India’s interests
- Effect of policies and politics of developed and developing countries on India’s interests, Indian diaspora.
India and US Strategic partnership
Should India please everyone or pursue its own interests?
- Recent visit of PM Modi to Washington D.C. resulted in signing of joint statement between India and US.
- However, as India consolidates the strategic partnership with the United States, there is a huge claim that it “tilts” India towards the U.S.
- Critics and doubters have questioned about the cost of becoming real friends with America.
Paradox situation: Critics argue that – ‘On one hand the joint statement may set out to advance substantive engagement with the U.S. (which is good) but on the other hand this new tilt may constrain India’s ability to conduct its diplomacy with other major powers like China and Russia (which is a concern)
But it is important to note that –
- “All major actions in the world of foreign policy, as elsewhere, have consequences; some intended and other unintended”.
- Some would use that fact to avoid any diplomatic action (adopting a “do-nothing” strategy). Some tend to neglect the impact of one’s actions and are surprised by the responses of others (adopting a “more decisively tilting” strategy).
Contemporary India has plenty of experience in both directions.
Case I : ‘do-nothing approach’
- We have witnessed the ‘do-nothing approach’ which the decade-long UPA rule adopted, which had resulted in poor diplomatic action and paralysed the UPA government including the potential loss of support from key political constituencies at home and the much-vaunted strategic autonomy abroad.
- The costs of do-nothing strategy are significant, as there were no significant trade agreements between India and USA nor India and Pakistan attained any good partnership.
Case II: ‘pursue your own interests’
- At the same time, India has experienced the dangers of moving decisively without anticipating the reactions or consequences. Delhi failed to anticipate the reactions of Pakistan, China and the West to a series of moves that Prime Minister Indira Gandhi made during 1971-75.
- Those bold moves – which included an alliance with the Soviet Union, breaking up Pakistan by liberating Bangladesh, conducting the first nuclear test, and integrating Sikkim into the Indian Union – resulted in some merits but the consequences was more severe.
The way ahead:
Pursue own interest but at the same time decisively broaden relations with all the major powers and deepen engagement with neighbours
Therefore, the Modi government has to be wary of these two-fold challenges (explained in Case I and II). India, while moving decisively to take full advantage of the entente with America, should also anticipate and manage some of the inevitable consequences of the new strategic warmth towards Washington.
The Modi government has to reassure its other partners in the international arena, especially Russia and China, who have some concerns about India’s relations with the United States. A similar effort will also be needed with our neighbours. In other words, India should broaden relations with all the major powers and deepen its engagement with neighbours.
Delhi must now broaden its diplomatic activism to reduce the potential costs and maximise benefits.
Connecting the dots:
- Critics argue that the new symphony in India-U.S. ties will limit New Delhi’s engagement with other world powers or emerging economies and acts as a threat to strategic autonomy. Do you agree? Substantiate your view.
NATIONAL
TOPIC: General Studies 2
- Issues relating to development and management of Social Sector or Services relating to Health, Education, Human Resources
Ensuring safe Blood—World Blood Donor Day
- Blood is a scarce resource and is also an essential element of human life, with no substitutes. In developing countries, blood transfusion services have traditionally been a low priority in health service development.
- Whatever the degree of development of the health care system, transfusion is the only option for survival for many patients. Thus, blood transfusion services occupy a vital space in any National Health Service delivery system. Safe transfusion requires not only the application of science and technology to blood processing and testing, but also require social mobilization to promote voluntary blood donation by people who have no infectious diseases that can be transmitted to the recipients of their blood.
Voluntary Vs. Replacement Donors:
Voluntary donors from low-risk populations form the cornerstone of a programme of safe and adequate blood supply; comprises only about 70 per cent of the demand in India, with the rest being met by replacement donation.
Statistics speak: Progressive increase in voluntary blood donation
- From about 54.5 per cent in 2006, the amount of blood collected from voluntary donors rose to 84 per cent in 2013-2014 in National AIDS Control Organisation (NACO)-supported blood banks.
- The total annual amount of units collected has also shown an absolute increase in over 10 years — from 4.4 million blood units in 2007 to 10 million units on average in the last three years
- The 1,161 NACO-supported blood banks alone accounted for over 5.7 million blood units collected during 2013-2014
- Least Voluntary donation of only 57 per cent— In Delhi; due to greater reliance on replacement donors and the more number of private sector blood banks.
- Reason for high collection—included family donors under the ambit of voluntary donation; however, in 2014, the definition of voluntary blood donation was modified in accordance to the WHO definition.
- Percentage of voluntary donations (2015-2016)— after excluding for family donors, was 79 per cent
Replacement Donors—A norm to be phased out “in a time bound programme”— WHY—
- Replacement donors are friends and relatives of a patient who donate blood as replacement for the blood given to the patient. Paid blood donation was banned in January 1998 but professional donors going ahead as the replacement donors have become the norm
- Many times, the recipients are harmed due to hiding or overlooking the many dont’s of donation
- Lack of initiative in studying their elaborate medical history and carrying out behavioural screening
Asian Journal of Transfusion Science (2012): Voluntary self-deferral to donate without citing reasons is widely accepted, replacement donors rarely resort to it either to hide their high-risk behaviour or due to pressure to meet the immediate demand for certain units of blood. As a result, the prevalence of HIV, hepatitis B, and hepatitis C is much higher among family donors when compared to voluntary donors
- Failure in detection: donated blood is screened for transfusion transmitted infections (TTI) such as HIV, hepatitis B, hepatitis C, syphilis and malaria; the tests fail to detect the diseases in the window period of infection. In the case of HIV, the window period (time between exposure to infection and the point when the test reflects accurate results) varies depending on the sensitivity and specificity of the assay used. Further, the risk of replacement donors having TTIs is 1.5-2.5 times higher than for voluntary donors.
- National Blood Policy of 2007 was formulated to shift the onus on institutions that prescribe blood for transfusions to procure blood for their patients from licensed banks. But Indian Journal of Medical Research revealed that nearly 97 per cent of donations made (2005-2013) at the Indraprastha Apollo Hospitals, Delhi, came from replacement donors.
Solution—
2015: National Blood Transfusion Council has decided to allow even hospital-based private blood banks to conduct donation camps. But there is a need to amend and notify Drugs and Cosmetics Act 1940 and Rules 1946.
Create awareness: Phasing out replacement donors & shifting of focus to increasing blood collection through voluntary donations to meet ‘over 95 per cent of blood requirement’
- Providing appropriate facilities for people to donate blood
- Improved donor retention
- Need to permit the bulk transfer of blood and blood components between blood banks
- Meet the National AIDS Control Programme IV (2012- 2017) plan of having in place over 50 per cent of all the blood banks that are NACO-supported and collect 90 per cent of the blood in the country, with 95 per cent of the donation from voluntary donors
The costs of Unsafe Blood
An unsafe or inadequate blood supply is even more costly – in both human and economic terms
- Morbidity and mortality resulting from the non-availability of blood or the transfusion of infected blood—direct impact on individuals and their families
- Transfusion of infected blood—an ever-widening pool of infection in the general population with far-reaching consequences for society as a whole
- Increased requirements for medical and social care, Loss of productive labour and higher levels of dependency—heavy burdens on overstretched health and social services and on national economies
The Action Plan on blood safety is driven by the need to continually improve and upgrade the availability and safety of blood and blood products, and to facilitate a self-sustaining national blood transfusion programme.
IASbaba’s Views:
The incidence of transfusion-transmitted infection – and its associated costs – will increase in countries that do not take stringent measures to ensure blood safety. Therefore, an investment in a safe and adequate blood supply is not only a responsibility of government, but also a cost-effective investment in the health and economic wealth of every nation. WHO recommends—
- A well-organized, nationally-coordinated blood transfusion service that can provide adequate and timely supplies of safe blood for all patients in need
- The collection of blood only from voluntary non-remunerated blood donors from low-risk populations
- Testing of all donated blood for transfusion-transmissible infections, blood grouping and compatibility testing
- The appropriate clinical use of blood, including the use of alternatives to transfusion wherever possible, and the safe administration of blood and blood products
- Quality system covering all stages of the transfusion process
Basic requirements for blood transfusion safety (WHO)—
Policy: National coordination of the blood programme is required to ensure uniform standards at all levels and facilitate economies of scale in testing and processing:
- National blood policy and plan
- Legislation and regulation
- Well-structured blood transfusion service (BTS)
- Specific budget allocation
- Standards for blood transfusion services
Quality and safety: The quality and safety of blood provided for patients depends not only on a national quality system for blood transfusion services, but quality in every activity. An effective national quality system requires:
- National quality policy and plan
- Quality officers at national and local levels
- Quality standards
- Documentation system
- Training of all staff
- Assessment of the quality system
Regular, voluntary non-remunerated blood donors from low-risk populations are the foundation of a safe blood supply—
- National blood donor programme
- Identification of low-risk donor populations
- National criteria for donor selection
- Safe blood collection procedures
- Donor notification and referral for counselling
- Donor records
Access: Provision should be made for a rapid response to emerging infections, emergency situations and post-disaster reconstruction.
MUST READ
Public land and private treatment
Breaking the Israel-Palestine logjam
Related Articles:
Palestine’s deepening occupation
U.N. accuses Israel, Hamas of committing war crimes
AIR – INDIA – ISRAEL, PALESTINE AND JORDAN
Latest Wave of Violence in the Hub of Cemeteries: Israel & Palestine
Dual diplomacy for Mission NSG
Related Articles:
Nuclear Suppliers Group – Mind Map
Quest for another Holy Grail – Nuclear Suppliers Group (NSG)
America’s new terror reality
Intolerant liberals?
Denying Ambedkar his due
Related Articles:
The Big Picture – B R Ambedkar: Mascot or Philosopher?
Why women want prohibition
Related Articles:
Of liquor bans and the ballot box
Kerala’s Liquor Policy: All in the spirit of equality
Gross Domestic Perplexity
Rains, reservoirs and food prices
Understanding bitcoins and blockchain
Related Articles:
How to deal with the corporate debt problem
MIND MAPS
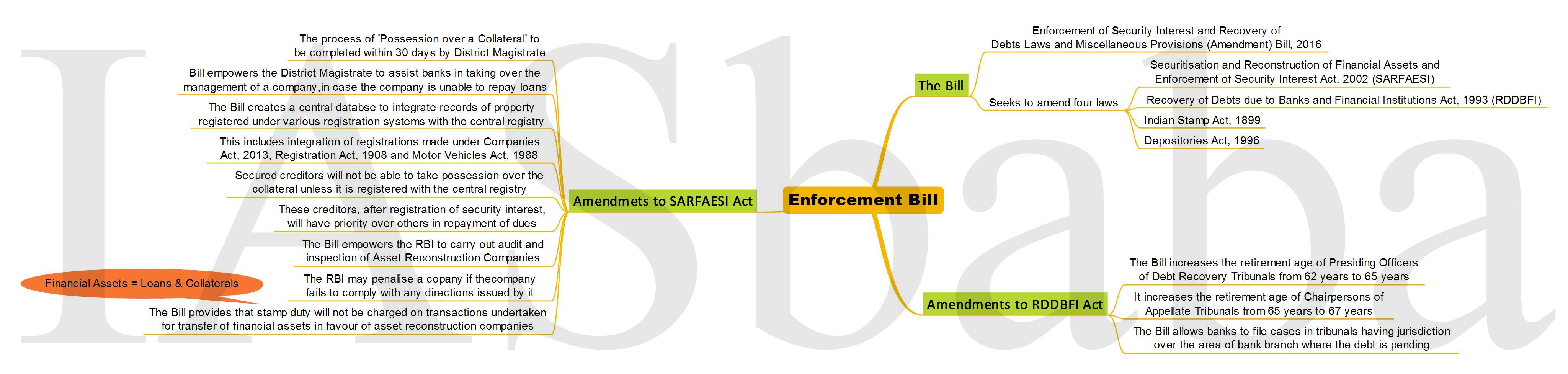
1. Enforcement Bill