Governance
Context:
- Rural Health is a state subject. Every state is responsible for raising the level of nutrition and the standard of living of its people and the improvement of public health as among its primary duties.
- Rural India is home to 68 per cent of India’s total population, and half of them live below the poverty line- struggling for better and easy access to health care and services.
- Health issues confronted by rural people are many and diverse ranging from severe malaria to uncontrolled diabetes from a badly infected wound to cancer.
- A huge improvement has been recorded when the government launched the National Rural Health Mission.
Rural healthcare system in India:
- The health care infrastructure in rural areas has been developed as a three tier system.
- As on March 2011, there are 148124 sub centres, 23887 Primary Health Centres and 4809 Community Health centres functioning in the country
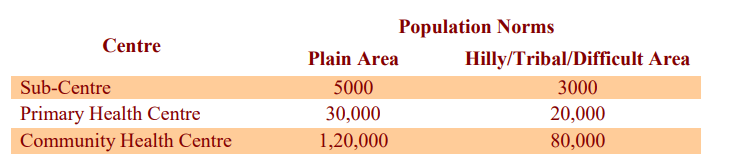
- In the Indian healthcare system, sub-centres (SC) are the first point of contact for a patient, catering to a population of 3,000-5,000.
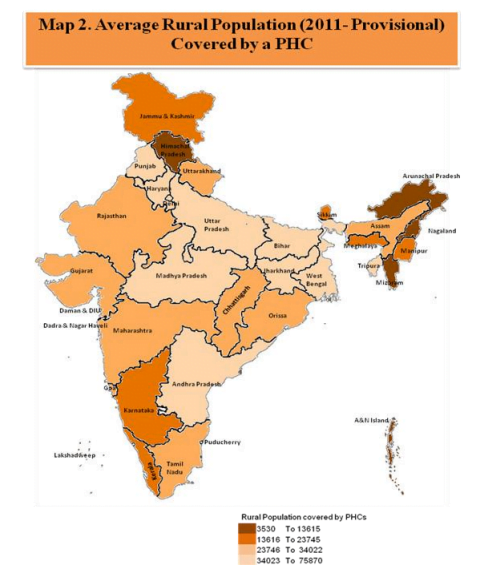
- This is succeeded by a PHC, which is required to look after the daily needs of 20,000-30,000 people.
- CHCs provide referrals and access to specialists, catering to 80,000-120,000 people.
- Urban PHCs — part of the National Health Mission’s efforts to set up multi-tier health centres caters to a population of 50,000-75,000
- Components of an effective healthcare system
- Availability of manpower
- Adequate infrastructure
- Robust policy framework
Challenges in India
- India’s rural healthcare system continues to be plagued by shortfall on two critical fronts — doctors and infrastructure.
- Shortage of qualified doctors– There is a shortage of 83.2 per cent of surgeons, 74.2 per cent of obstetricians and gynaecologists, 79.1 per cent of physicians and 81.6 per cent of paediatricians, according to the Rural Health Statistics 2021-2022 released last week.
- The number of doctors at PHCs has shrunk to 30,640 in 2022 from 31,716 in 2021. Lab technicians, nursing staff and radiographers at PHCs and CHCs have all recorded a marginal increase between 2021 and 2022. Up from 22,723 to 22,772, from 79,044 to 79,933 and from 2,418 to 2,448, respectively.
- Uttar Pradesh, Rajasthan, Madhya Pradesh, Gujarat and Odisha face the highest shortage in surgeons, obstetricians / gynaecologists, paediatricians and radiographers at CHCs across the country.
- Poor infrastructure – Less than half the Primary Health Centres (PHC), 45.1 per cent, function on a 24×7 basis. Of the 5,480 functioning Community Health Centres (CHC), only 541 have all four specialists
- Overburdened facilities – PHCs are overburdened across the board, with SCs currently looking after more than 5,000 people, PHCs catering to 36,049 people and CHCs to 164,027 people. This, coupled with a human resource shortage, plagues access to adequate and quality healthcare.
- Low number of support staff – The number of auxiliary nurse midwives at SCs has decreased to 207,587 in 2021 from 214,820 in 2022. The shortage was most pronounced in Uttar Pradesh, Gujarat, Himachal Pradesh, Odisha and Uttarakhand.
National Rural Health Mission (NRHM)
- The National Rural Health Mission (2005-12) seeks to provide effective healthcare to rural population throughout the country with special focus on 18 states, which have weak public health indicators and/or weak infrastructure such as Arunachal Pradesh, Assam, Bihar, Chhattisgarh, Himachal Pradesh, Jharkhand, Jammu & Kashmir, Manipur, Mizoram, etc.
- The Mission is an articulation of the commitment of the Government to raise public spending on Health from 0.9% of GDP to 2-3% of GDP.
Objectives of NRHM
- Architectural correction of the health system to enable it to effectively handle increased allocations as promised under the National Common Minimum Programme and promote policies that strengthen public health management and service delivery in the country.
- Provision of a female health activist in each village; a village health plan prepared through a local team headed by the Health & Sanitation Committee of the Panchayat
- Train and enhance capacity of Panchayati Raj Institutions (PRIs) to own, control and manage public health services
- Promote access to improved healthcare at household level through the female health activist (ASHA)
- Integration of vertical Health & Family Welfare Programmes, optimal utilization of funds & infrastructure, and strengthening delivery of primary healthcare.
- It seeks to revitalize local health traditions and mainstream AYUSH into the Community Health Centre (CHC)
- It seeks decentralization of programmes for district management of health and to address the inter-State and inter-district disparities
- It also seeks to improve access of rural people, especially poor women and children, to equitable, affordable, accountable and effective primary healthcare.
Achievements:
- The allopathic doctors at PHCs have increased from 20,308 in 2005 to 30,640 in 2022, which is about 50.9% increase.
- The specialist doctors at Community Health Centers (CHCs) have increased from 3,550 in 2005 to 4,485 in 2022
Other healthcare schemes:
Reproductive, Maternal, Neonatal, Child and Adolescent health
- Universal Immunisation Programme
- Mission Indradhanush (MI)
- Janani Suraksha Yojana (JSY)
National Nutritional Programmes
- National Iodine Deficiency Disorders Control Programme
- MAA (Mothers’ Absolute Affection) Programme for Infant and Young Child Feeding
Communicable diseases
- National AIDS Control Programme (NACP)
- Pulse Polio Programme
Non-communicable diseases
- National Tobacco Control Programme(NTCP)
- National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases & Stroke (NPCDCS)
- National Mental Health Programme
Way forward
- Recently, the government has scrapped custom duties on drugs and test kits used to treat AIDS in an effort to cut prices across the country.
- With a policy to double spending on health and devise innovative methods of health management there is renewed hope that the people of the country will have greater access to facilities and be healthier.
- The promise of Health Assurance is an important catalyst for the framing of a New Health Policy in a developing India.
Source: DTE