- Home
- UPSC Mains
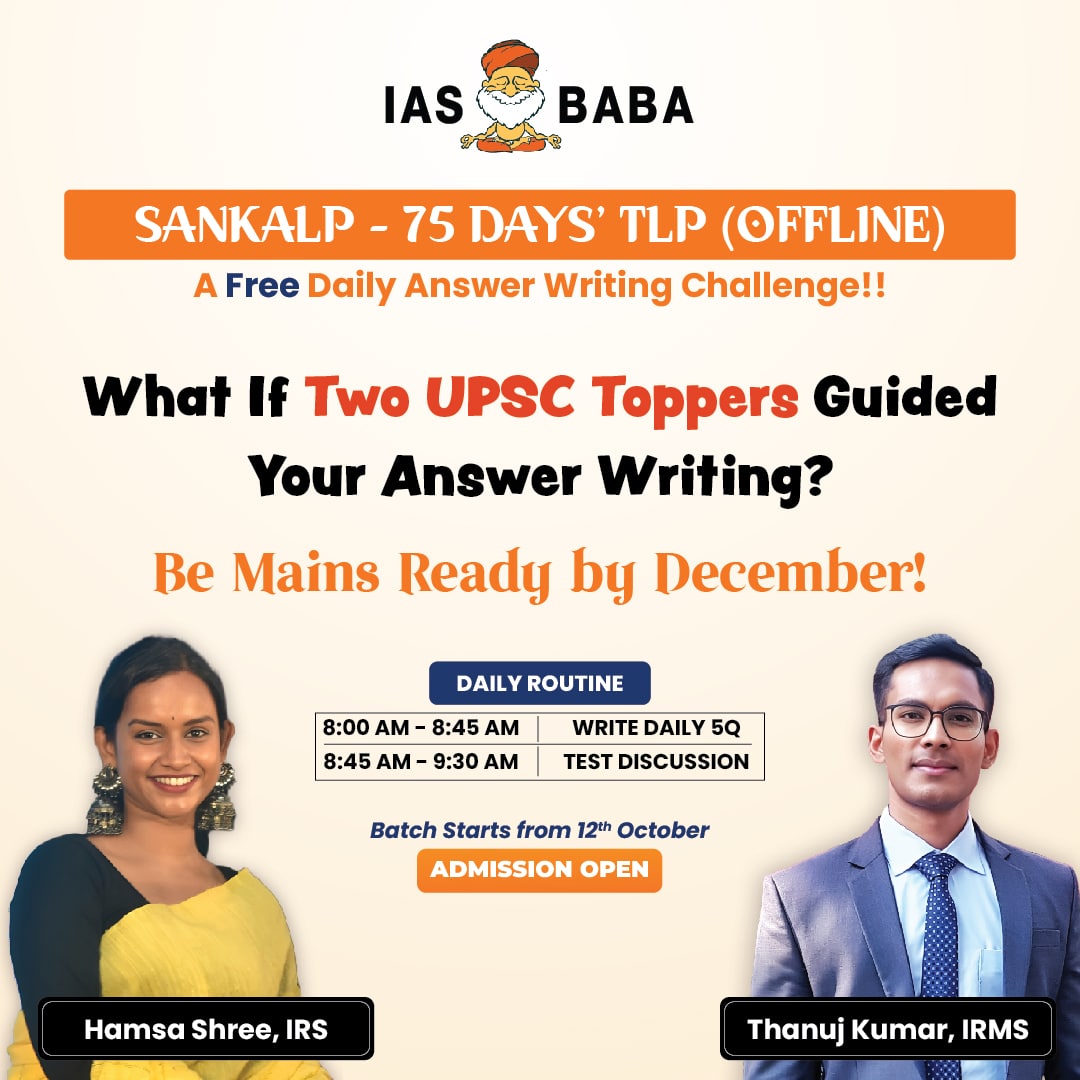
- Daily Free Initiatives
- Courses
- CSAT Mastery – 20 Days’ Smart Practice Programme
- SUPER 50: 1:1 Mentorship Programme Under Mohan Sir
- Prelims Exclusive Mentorship Programme – PEP 2026
- Integrated Learning Program (ILP) – 2026
- Think Learn Perform (TLP) Connect for UPSC 2026
- Baba’s Gurukul Course – 2027
- UPSC 2025 Mains
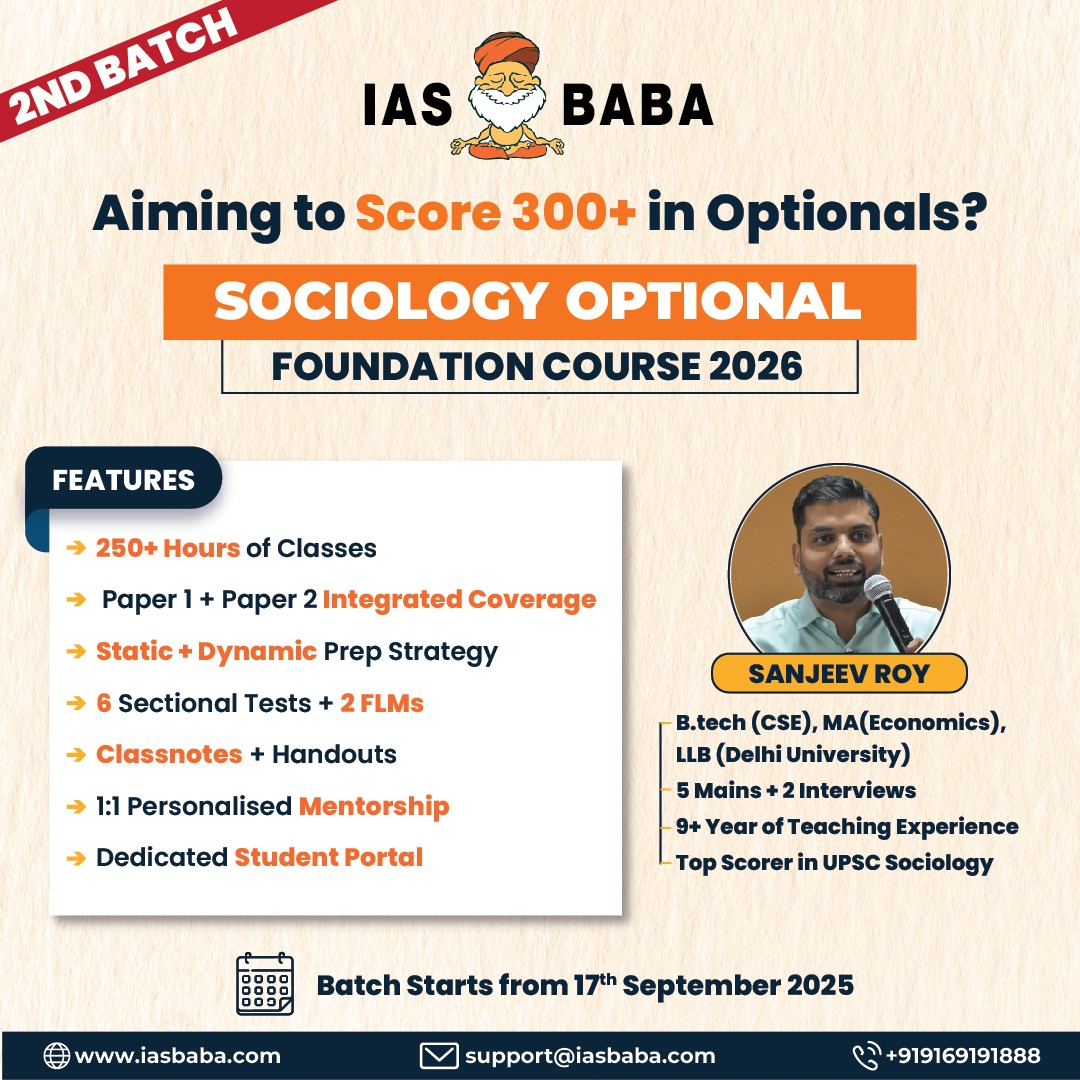
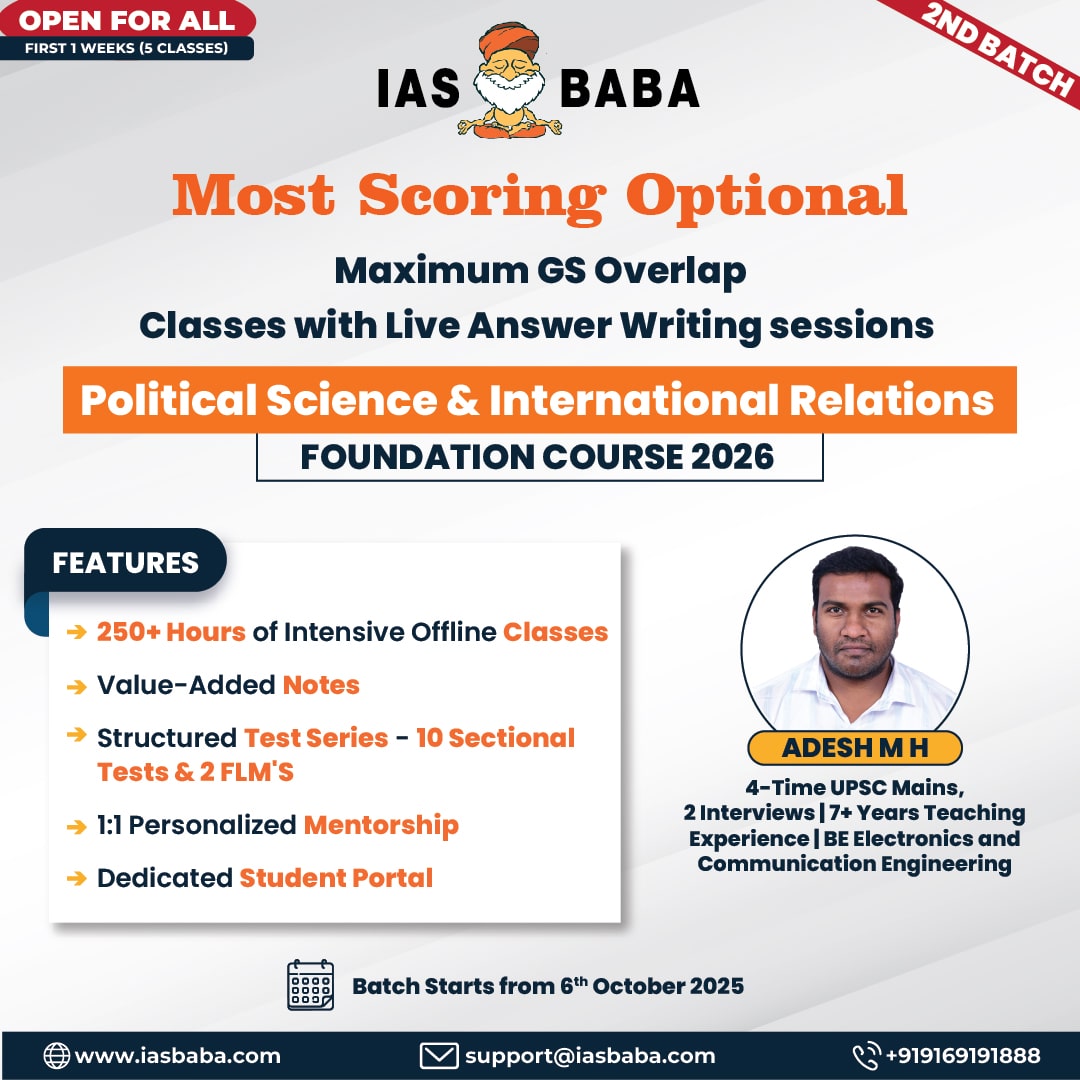
- Optionals
- KPSC / KAS
- हिंदी
- Centres
- Contact Us